WASHINGTON (Reuters) – U.S. law enforcement officials have charged 21 people across the country with healthcare schemes amid the pandemic as part of the administration’s larger effort to thwart people from leveraging COVID-19 for fraud, the Department of Justice said on Wednesday.
The latest charges include cases involving filing false Medicare and other billing claims, kickbacks and money laundering, the department said, adding the alleged actions led to more than $149 million in COVID-19-related false billings to federal programs and theft from federally-funded pandemic assistance programs.
More than $8 million in cash and other fraud proceeds were able to be recovered, it said in a statement.
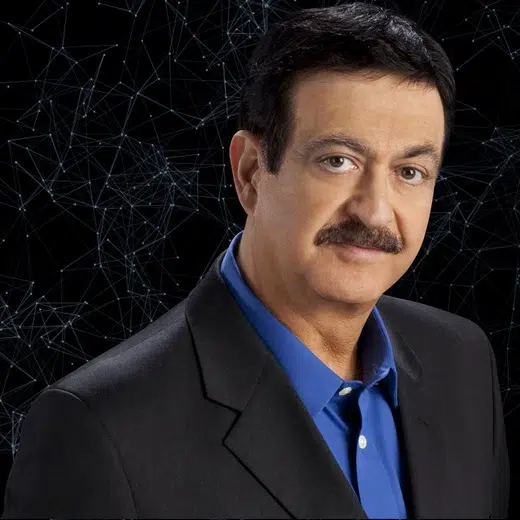
“Throughout the pandemic, we have seen trusted medical professionals orchestrate and carry out egregious crimes against their patients all for financial gain,” Luis Quesada, assistant director of the Federal Bureau of Investigation’s Criminal Investigative Division, said.
Others were charged with manufacturing and distributing fake COVID-19 vaccine record cards, it added.
The Centers for Medicare & Medicaid Services separately said it had taken 28 administrative actions against healthcare providers for their alleged fraud, according to the Justice Department.
The department last month tapped a federal prosecutor to lead the COVID-related anti-fraud efforts, saying such probes were a top priority.
As of late March, Justice officials said they had brought more than 1,000 criminal cases as part of its pandemic enforcement efforts.
(Reporting by Susan Heavey; Editing by Tomasz Janowski)